Scientists at Washington University School of Medicine in St. Louis develop a nanoparticle that can deliver chemotherapy directly to tumour cells that have spread to bone. Animal tests show, the treatment kills tumour cells and reduces bone destruction while sparing healthy cells from side effects in mince implanted with human breast cancer.
Washington (ISJ) – Breast cancer that spreads often infiltrates bone, causing fractures and intense pain. In such cases, chemotherapy is ineffective because the environment of the bone protects the tumour, even as the drug has toxic side effects elsewhere in the body.
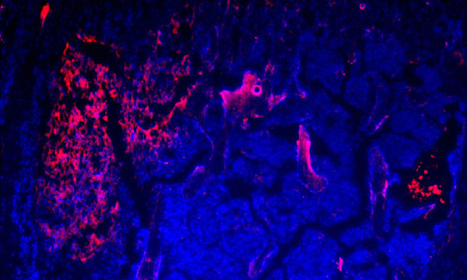
Now, scientists at Washington University School of Medicine in St. Louis have developed a nanoparticle that can deliver chemotherapy directly to tumour cells that have spread to bone. In mice implanted with human breast cancer and exposed to circulating cancer cells likely to take up residence in bone, the researchers showed the treatment kills tumour cells and reduces bone destruction while sparing healthy cells from side effects.
The study is available online in the journal Cancer Research.
“For women with breast cancer that has spread, 70 percent of those patients develop metastasis to the bone,” said senior author Katherine N. Weilbaecher, MD, a professor of medicine. “Bone metastases destroy the bone, causing fractures and pain. If the tumours reach the spine, it can cause paralysis. There is no cure once breast cancer reaches the bone, so there is a tremendous need to develop new therapies for these patients.”
In the study, the researchers showed that breast cancer cells that spread to bone carry molecules on their surface that are a bit like Velcro, helping tumour cells stick to the bone. These adhesion molecules also sit on the surface of cells responsible for bone remodelling, called osteoclasts.
“In healthy bones, osteoclasts chew away old, worn out bone, and osteoblasts come in and build new bone,” said Weilbaecher, who treats patients at Siteman Cancer Centre at Barnes-Jewish Hospital and Washington University School of Medicine. “But in cancer that spreads to bone, tumours take over osteoclasts and essentially dig holes in the bone to make more room for the tumour to grow.”
Weilbaecher said she and her colleagues were surprised to find that the same adhesive molecule on the surface of osteoclasts also is present in high levels on the surface of the breast tumours that spread to bone. The research showed that the molecule — called integrin αvβ3 — was absent from the surfaces of the original breast tumour and from tumours that spread to other organs, including the liver and the lung. The researchers confirmed that this pattern also was true in biopsies of human breast tumours that had spread to different organs.
Weilbaecher collaborated with Gregory M. Lanza, MD, PhD, a professor of medicine and of biomedical engineering, which led to the design of a nanoparticle that combines the bone-adhesion molecules with a form of the cancer drug docetaxel, which is used to treat breast cancer as well as other tumours. Lanza is the senior co-author of the study.
The adhesive molecules allow the nanoparticle to penetrate the otherwise protective environment of the bone matrix in a way that, in essence, mimics the spreading of the tumour cells themselves. The result is a delivery method that keeps the chemotherapy drug contained in the nanoparticle until the adhesion molecules make contact with the tumour cell, fusing the nanoparticle with the cell surface and releasing the drug directly into the cancer cell.
“When we gave these nanoparticles to mice that had metastases, the treatment dramatically reduced the bone tumours,” Weilbaecher said. “There was less bone destruction, fewer fractures, less tumour. The straight chemo didn’t work very well, even at much higher doses, and it caused problems with liver function and other toxic side effects, which is our experience with patients. But if we can deliver the chemo directly into the tumour cells with these nanoparticles that are using the same adhesive molecules that the cancer cell uses, then we are killing the tumour and sparing healthy cells.”